
The Menopause Transition, Vaginal Health, and Your Vaginal Microbiome
This article is part of The Vaginal Biome Hub - a science-backed content series from Daye and Twentyeight Health, reframing menopause not as decline, but as evolution. Together, we’re translating the latest research into tools that help people move through menopause with agency, comfort, and clarity.
How Menopause Transforms Vaginal Health and the Vaginal Microbiome
Menopause doesn’t simply mark the end of menstruation. It’s a whole-body transition that reshapes hormones, metabolism, tissues - and the microscopic ecosystem that lives within your vagina - your vaginal microbiota.
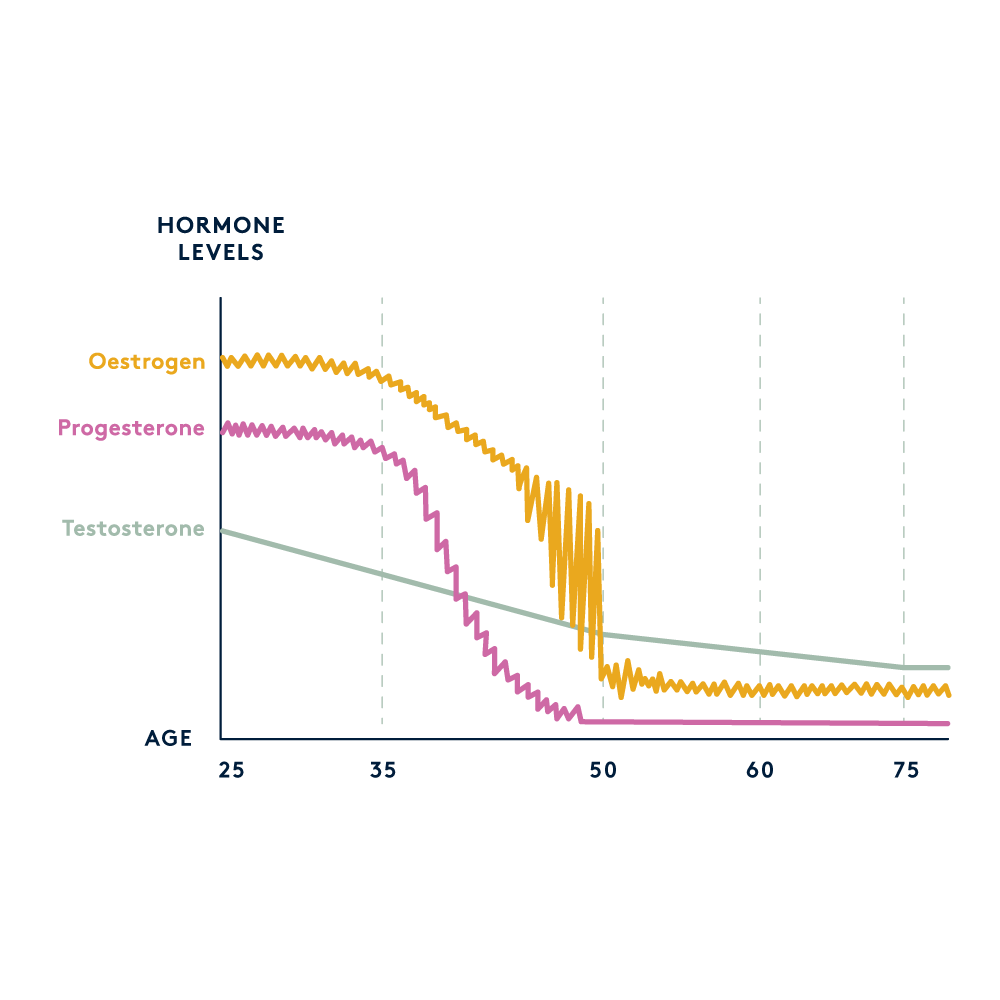
During your reproductive years, estrogen plays a quiet but crucial role: it fuels the vaginal lining’s glycogen stores. Glycogen is a natural form of stored sugar your body uses for energy - but in the vagina, it’s the primary food source for Lactobacilli, the “good” bacteria that maintain your microbial balance. Lactobacilli breaks down glycogen into lactic acid, which keeps the vaginal pH between 3.8 and 4.5, making it acidic enough to protect against pathogens, inflammation, and dryness.
When estrogen levels drop during perimenopause, glycogen supplies decline. The Lactobacilli lose their food source, lactic acid production slows, and the vaginal pH rises. As your environment becomes less acidic, anaerobic bacteria - species like Gardnerella or Prevotella, which cause bacterial vaginosis that thrive without oxygen - begin to multiply. This subtle microbial shift is what sets the stage for dryness, itching, pain during sex, and more frequent vaginal or urinary infections, which we associate with the peri(menopause) transition.
Additionally, new research suggests the connection goes both ways: the vaginal microbiome might also metabolize hormones locally, influencing how estrogen and progesterone behave in the vaginal tissue. In essence, your microbes don’t just respond to your hormones - they help shape them. This may explain why some people experience vaginal (peri)menopause symptoms even when blood hormone levels appear normal.
Hormones, the Vaginal Lining, and Comfort
When estrogen dips, the vaginal tissue becomes thinner, less elastic, and less lubricated. This condition, known as Genitourinary Syndrome of Menopause (GSM), can cause burning, pain with sex, or a feeling of tightness. The urethra — the small tube that carries urine — is affected too, which is why urinary tract infections (UTIs) often become more frequent after menopause.
The culprit isn’t just low estrogen; it’s also microbial imbalance. When protective Lactobacilli decline alongside estrogen and progesterone, bacteria from the gut or urinary tract — such as E. coli — can more easily take hold. Likewise, bacterial vaginosis (BV) becomes more common post-menopause because the loss of vaginal acidity lets opportunistic pathogens flourish. BV and UTIs often appear together, reflecting a broader microbiome imbalance that connects the vagina, bladder, and urinary tract.
Understanding this triad — hormones, microbes, and mucosa — is essential for lasting comfort. Menopause symptoms aren’t just hormonal; they’re very connected to the vaginal microbiota.
Caring for Your Vaginal Microbiome During Perimenopause
Many of these changes are reversible — or at least manageable — once you understand what’s happening and take action early. One of the most effective and well-studied tools we have is hormone support. Vaginal tissues are exquisitely hormone-responsive, and even small corrections — especially with local estrogen — can transform comfort, microbiome stability, and sexual wellbeing.
1. Support your hormones, locally and gently.
Declining estrogen is the single most important driver of vaginal microbiome disruption during perimenopause. When estrogen falls, glycogen stores thin out, vaginal pH rises, and Lactobacilli lose their primary food source — setting the stage for dryness, pain, and recurrent infections.

Low-dose vaginal estrogen (available as a cream, ring, or tablet) directly reverses this. It rebuilds the vaginal lining, restores glycogen, lowers pH, and enables Lactobacilli to return and re-stabilize the microbiome. Because it’s applied locally, it acts where it’s needed and enters the bloodstream in extremely small amounts.
And importantly: the FDA recently removed the boxed warning on low-dose vaginal estrogen products after reviewing extensive safety data. This shift reflects what menopause specialists have said for years: local estrogen is safe for the vast majority of people, even long-term, and it’s one of the most effective treatments for vaginal and urinary symptoms in midlife.
If you’re experiencing dryness, pain with sex, urinary urgency, recurrent infections, or a loss of natural lubrication, this is often the most direct path to relief.
2. Rebuild your bacterial defenders.
If estrogen isn’t an option, certain probiotics — particularly Lactobacillus crispatus, L. rhamnosus, and L. plantarum — have been shown to lower vaginal pH and support tissue resilience. You can find these strains in oral or vaginal supplements, just make sure you select live, clinically-tested cultures.
3. Nourish your microbes and hydrate your tissues.
Your vaginal microbiome depends on what you feed it. Lactobacilli flourish when your diet includes fiber and fermented foods — think kefir, kimchi, sauerkraut, or yogurt — all rich in live cultures that help balance gut and vaginal bacteria. Hydration matters just as much: well-hydrated mucosal tissue stays supple, making it easier for beneficial microbes to colonize and protect.
A quick hydration check? Look at your urine. Pale yellow usually means you’re well hydrated; darker tones signal you need more fluids. But if your urine is completely clear, you may be overdoing it — too much water can dilute your body’s natural electrolytes and affect overall wellbeing.
4. Protect your pH.
Avoid perfumed soaps, fragranced tampons or pads, vaginal douching, and overly alkaline washes. Opt for gentle, pH-balanced products and natural lubricants that won’t disrupt acidity. After sex, rinse the vulva with warm water and avoid harsh cleansers that strip away good bacteria. Never wash inside your vaginal canal. Remember, the vagina is self-cleaning thanks to your Lactobacilli.
5. Stay curious, not resigned.
If you notice new symptoms — burning, itching, odor, or recurrent infections — don’t chalk them up to “just menopause.” A simple vaginal microbiome test, like Daye’s at-home kit, can identify whether you’ve lost Lactobacilli or developed BV-associated bacteria. Once you know the cause, solutions become clear.
Daye’s diagnostic platform gives you insight into your microbial health, while Twentyeight Health offers discreet access to vaginal estrogen therapy, probiotics, and menopause care consultations — making it easier to take control of your comfort, wherever you are in your transition.
The Future of Menopause Care
Menopause isn’t the end of fertility — it’s the beginning of microbial adaptation. The vaginal microbiome you had at 30 won’t be the same at 55, and that’s okay. What matters is maintaining equilibrium.
At The Vaginal Biome Hub, Daye and Twentyeight Health are exploring the intersection of microbial science, hormonal biology, and patient experience. Our shared goal is simple: to make precision vaginal health care accessible at every stage of life. Because the same principle applies across the decades — when you nurture your microbes, they nurture you back.
Menopause – The natural life stage when menstrual periods have stopped for at least 12 months, marking the end of ovarian hormone production. Typically occurs between ages 45 and 55.
Perimenopause – The transition period before menopause when estrogen and progesterone levels fluctuate, often causing irregular periods, hot flashes, and changes in vaginal health.
Estrogen – The primary female sex hormone that supports vaginal thickness, elasticity, blood flow, and Lactobacilli growth by increasing glycogen stores.
Glycogen – A storage form of sugar in vaginal cells. Estrogen stimulates its production, and Lactobacilli metabolizes it into lactic acid to maintain a low, protective pH.
Lactobacilli – Beneficial bacteria that dominate a healthy vaginal microbiome. They lower pH, produce hydrogen peroxide, and protect against BV, yeast infections, and UTIs.
Anaerobic bacteria – Microbes that thrive in low-oxygen environments. In menopause, they can overgrow when Lactobacilli decline, increasing infection and odor risk.
Bacterial vaginosis (BV) – A common imbalance where harmful bacteria replace Lactobacilli. More frequent after menopause due to reduced acidity.
UTIs (Urinary Tract Infections) – Infections of the urinary system often linked to a depleted vaginal microbiome and bacterial migration from the vagina or gut.
Genitourinary Syndrome of Menopause (GSM) – A set of symptoms including vaginal dryness, burning, pain with sex, and urinary urgency caused by low estrogen and microbiome disruption.