
This article is part of The Vaginal Biome Hub - a collaboration between Daye and Twentyeight Health, created to bring proper science and practical care into everyday vaginal health. In this piece, we’re untangling the vaginal infections many of us experience constantly yet often struggle to get meaningful guidance on.
Your vagina is home to a dynamic community of microbes that constantly negotiate with your hormones, immune system, and daily habits. Most days, this community stays balanced thanks to high Lactobacilli counts - the good bacteria that keep the vaginal environment slightly acidic and hostile to troublemakers (a.k.a. pathogens, which cause infections). But even relatively small shifts in hormones, immunity, stress, sex practices, or medication can push this equilibrium off-kilter. When it does, yeast and bacterial vaginosis (BV) tend to step into the spotlight.
These conditions aren’t signs of poor hygiene or neglect. They’re the natural consequence of a microbiome that’s responding to internal and external pressures. Understanding that alone can be liberating for many, especially those that have been shamed for decades by the “feminine hygiene” industry.
Yeast: A Normal Resident That Takes Over When Your Defenses Drop
Yeast - usually Candida albicans - is meant to live in the vagina in small amounts. It only becomes a problem when it multiplies faster than your Lactobacilli can keep it in check. This often happens after a course of antibiotics, which wipe Lactobacilli out; during high-estrogen phases of the menstrual cycle; or when your immune system is under strain. Even irritation from fragranced products or synthetic (non-cotton) underwear + legging fibres can disrupt the balance enough to allow yeast to flourish.
The symptoms vary more than people expect. Intense itching is common, but some people experience only mild irritation, and discharge can be thick, thin, or barely visible. This variability is why so many people misdiagnose themselves - studies show that nearly half of self-diagnosed “yeast infections” aren’t yeast at all.
Accurate diagnosis matters, and that’s where Daye’s vaginal microbiome test becomes genuinely useful. Instead of guessing, you can see whether yeast is truly the culprit or whether your symptoms have an entirely different cause.
BV: The Microbiome’s Version of Losing Home Court Advantage
BV occurs when Lactobacilli diminish and anaerobic bacteria - such as Gardnerella, Prevotella, and Atopobium - begin to dominate. This shift changes vaginal pH, and opens the door to inflammation and infection.
BV has a reputation for causing odor, but not everyone experiences that. Some people notice only subtle changes in discharge or mild discomfort. Others have no symptoms at all and only discover the imbalance during routine testing. BV is often recurrent, not because treatments fail, but because the vaginal microbiome isn’t given a chance to rebuild itself properly afterward. Clearing the overgrowth is only step one; restoring Lactobacilli is step two, and that’s the step most people never get support with.
Twentyeight Health providers can help patients who have cycled through multiple rounds of BV treatment without long-term relief, simply because no one explained how to rebuild the protective bacteria once the anaerobes were reduced.
Yeast or BV? The Symptoms Don’t Always Tell the Truth
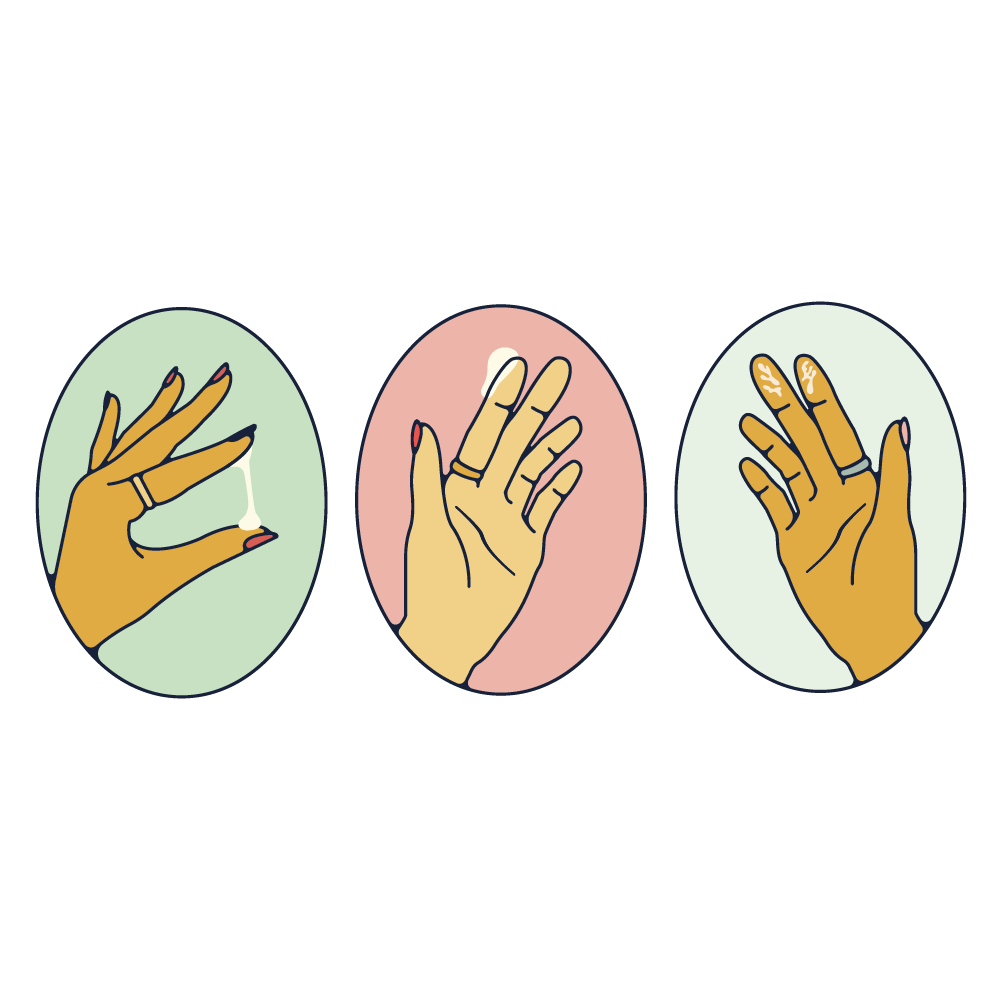
Many people try to diagnose themselves based on discharge or sensation alone, but the overlap between yeast and BV is more confusing than most guides suggest. Yeast tends to cause itching, redness, and soreness, while BV often alters pH and causes a thinner discharge with a stronger smell, especially after sex. Yet plenty of patients experience versions of these conditions that don’t follow the textbook at all.
To complicate matters further, mixed infections - yeast and BV at the same time - are surprisingly common. They require different treatments, so self-diagnosing based on “what it feels like” can easily lead you in the wrong direction. The most reliable way to know what’s happening is to look at the microbial landscape directly, which is exactly what Daye’s test is designed to do.
So What Actually Helps? Here’s What the Microbiome Responds To
The most important first step is identifying what’s happening before deciding how to treat it. Once you have clarity, the path forward becomes much easier.
Testing before treating isn’t overkill - it prevents unnecessary medications, avoids worsening symptoms, and gives you a clear plan. Daye’s at-home test makes this straightforward, and Twentyeight Health’s can help you interpret the results and choose the right medications or follow-up care.

After treatment, the vaginal ecosystem needs help rebuilding its Lactobacilli. This isn’t something that happens automatically, especially after antibiotics. Strains like Lactobacillus crispatus, L. rhamnosus, and L. plantarum are well-studied for supporting acidity and helping the microbiome return to a stable state, and both Daye and Twentyeight Health offers access to clinically validated probiotics that can support this reset.
Your daily environment also matters more than you think. High-pH washes, scented pads and tampons, and certain lubricants can make it harder for Lactobacilli to thrive. The vagina cleans itself internally and doesn’t require soap or douching; the vulva simply needs gentle care. Water or a mild, pH-balanced cleanser is enough - anything more is likely to cause more harm than good.
Timing also plays a role. Many people notice patterns - infections may occur after sex without a condom, during certain phases of the menstrual cycle, after changing contraception, or during stressful periods. These aren’t moral failings or hygiene mistakes; they’re biological responses to shifting pH, hormones, and immune activity.

Your vaginal microbiome also pays attention to your overall health. Sleep, stress, diet, and gut health all influence vaginal immunity. Supporting your general wellbeing is the foundation for microbial resilience.
The Real Goal Is Stability, Not Perfection
There’s no single “ideal” microbiome. Some vaginas prefer a crispatus-dominant ecosystem; others naturally contain more species. Some fluctuate with hormones, while others stay mostly steady. What matters is stability - an environment where Lactobacilli can hold their ground and protect the tissue, regardless of the curveballs your life throws at you.
Daye helps you understand what your microbiome is actually doing. Twentyeight Health helps you act on that information with evidence-based care. Together, we’re making vaginal health less of a guessing game and more of a supported, informed journey.
Your vagina isn’t fragile. It’s responsive, adaptable, and often trying to tell you exactly what it needs - once you learn how to read the signs.
Glossary
Bacterial Vaginosis (BV)
A common vaginal condition caused by a shift in the microbiome where protective Lactobacilli decrease and anaerobic bacteria multiply. BV often leads to an increase in vaginal pH, changes in discharge, and sometimes odor.
Candida (Yeast)
A fungus that naturally lives in small amounts in the vagina, gut, and skin. When it multiplies quickly - often after antibiotics, hormonal changes, or immune dips - it can cause itching, redness, swelling, and discomfort. Yeast infections are not caused by sex or hygiene habits.
Lactobacilli
Beneficial bacteria that dominate a healthy vaginal microbiome. They keep the vagina acidic by producing lactic acid, hydrogen peroxide, and other protective substances. High levels of Lactobacilli are strongly linked to lower rates of BV, yeast infections, HPV persistence, and other reproductive health concerns.
Vaginal pH
A measure of how acidic or alkaline the vagina is. A healthy vaginal pH typically ranges from 3.8 to 4.5, which keeps harmful bacteria in check. Semen, menstrual blood, antibiotics, and certain products can temporarily raise pH, sometimes triggering symptoms.
Anaerobic bacteria
Microbes that thrive in low-oxygen environments and often increase during BV. Common anaerobes include Gardnerella, Prevotella, and Atopobium. When they overgrow, they raise vaginal pH and can cause inflammation or odor.
Mixed infection
A condition where yeast and BV-associated bacteria are present at the same time. Mixed infections require tailored treatment because antifungals do not address BV and antibiotics do not address yeast.
Microbiome test
A diagnostic tool that analyzes which bacteria and yeast are present in the vagina and in what quantities. This helps distinguish between BV, yeast infections, mixed infections, and other imbalances and can support targeted, effective treatment.