If you’re of reproductive age, menstrual health is probably always on your mind. Periods are a regular part of life, showing up once a month—sometimes on time, sometimes late—and often bringing cramps, bloating, fatigue, and mood changes.
But your period isn’t just bleeding. It’s a full-body inflammatory event influenced by the trillions of microbes in your gut and vagina. Research shows these microbes affect how strong your cramps are, how heavy your bleeding is, and even your risk for vaginal infections.
This means your period pain—the cramps that have you reaching for a hot water bottle and a painkiller—isn’t only in your uterus. It can begin with bacteria in your gut and vagina.
While it’s tempting to focus only on relieving cramps, it’s important to know that gut health and periods are connected, as are periods and vaginal health. Let’s dive into the link between menstruation and the microbiome (gut and vaginal) to help make periods a little easier.
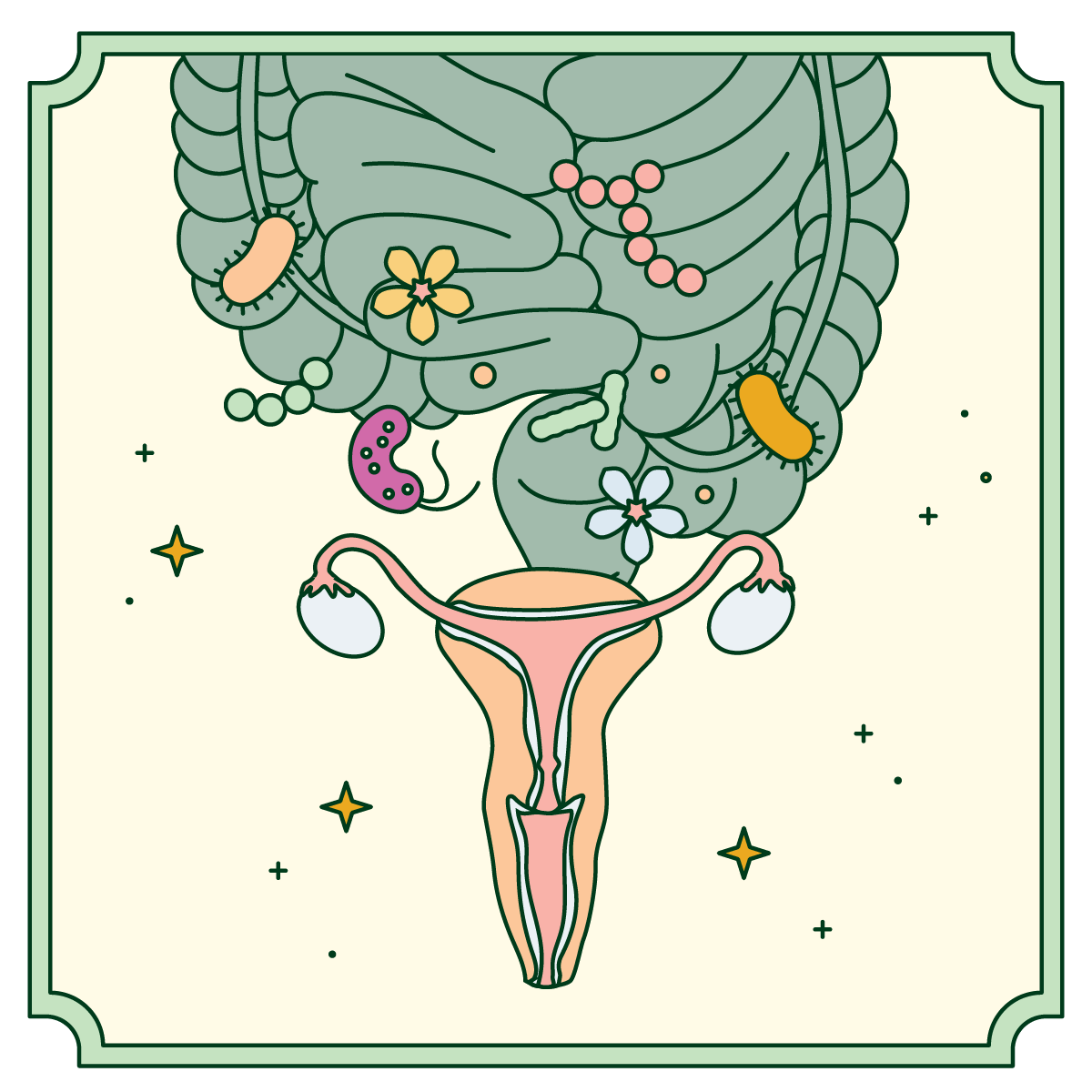
Your gut microbiome regulates estrogen through the estrobolome, bacterial genes that control how estrogen is broken down and reused. When the gut is unbalanced, estrogen clearance slows. This can lead to estrogen dominance, which is linked to heavier bleeding, breast tenderness, mood swings, and stronger cramps.
Studies show that changes in gut bacteria and high β-glucuronidase activity correlate with endometriosis and severe period pain (dysmenorrhea) severity. Think of your gut microbes as a recycling system for estrogen—if the system fails, estrogen builds up, and your period feels the impact.
Whether you call it “gut health and hormones,” “gut health and periods,” or “gut health and hormone imbalance,” it’s all connected, and it’s worth knowing.
“Menstruation is marked by increased vaginal microbial diversity and reduced Lactobacillus,” says Kecia Gaither, MD, Director of Perinatal Services/Maternal Fetal Medicine at NYC Health + Hospitals/Lincoln.
Lactobacilli are the “good bacteria” that keep the vagina healthy. When they decrease, the risk of infections like bacterial vaginosis (BV) or yeast infections rises—even before your period starts.
“When estrogen drops before and during menstruation, glycogen production in the vaginal lining decreases,” Dr. Gaither explains. “Lactobacilli converts glycogen into lactic acid, which keeps the vaginal pH acidic and protective. Lower estrogen means less glycogen, less lactic acid, and fewer Lactobacilli, making the vaginal environment more vulnerable to harmful bacteria.”
Period blood also affects vaginal health. Menstrual blood has a higher pH than normal vaginal conditions. When blood touches the vaginal lining, it temporarily raises pH, reducing Lactobacilli and allowing other bacteria to grow.
Dr. Gaither adds that the vaginal microbiome usually returns to normal about three days after menstruation ends. But poor menstrual hygiene—like leaving products in too long or not washing hands—can disrupt the microbiome and increase infection risk.
Rarely, toxic shock syndrome (TSS) can occur from bacterial infections caused by staph or strep bacteria. To reduce risk, it’s important to change tampons every 4–8 hours and alternate with pads. Daye tests their tampons to ensure they don’t promote harmful bacteria growth.
When Lactobacilli levels drop, it can cause more than infections—it may increase inflammation and pain signaling. Dr. Chen at the University of Arizona found that people with more pro-inflammatory bacteria often report severe cramps, while those with more Lactobacilli experience milder symptoms.
Pain can also spread to other pelvic organs like the bladder or bowel—a phenomenon called cross-organ sensitivity. Inflammatory bacteria in the vagina can trigger immune responses that affect nearby tissues, creating a cycle of pain and inflammation.
This research is promising. Conditions like endometriosis, which cause chronic pelvic pain, may improve by supporting a healthy vaginal microbiome.
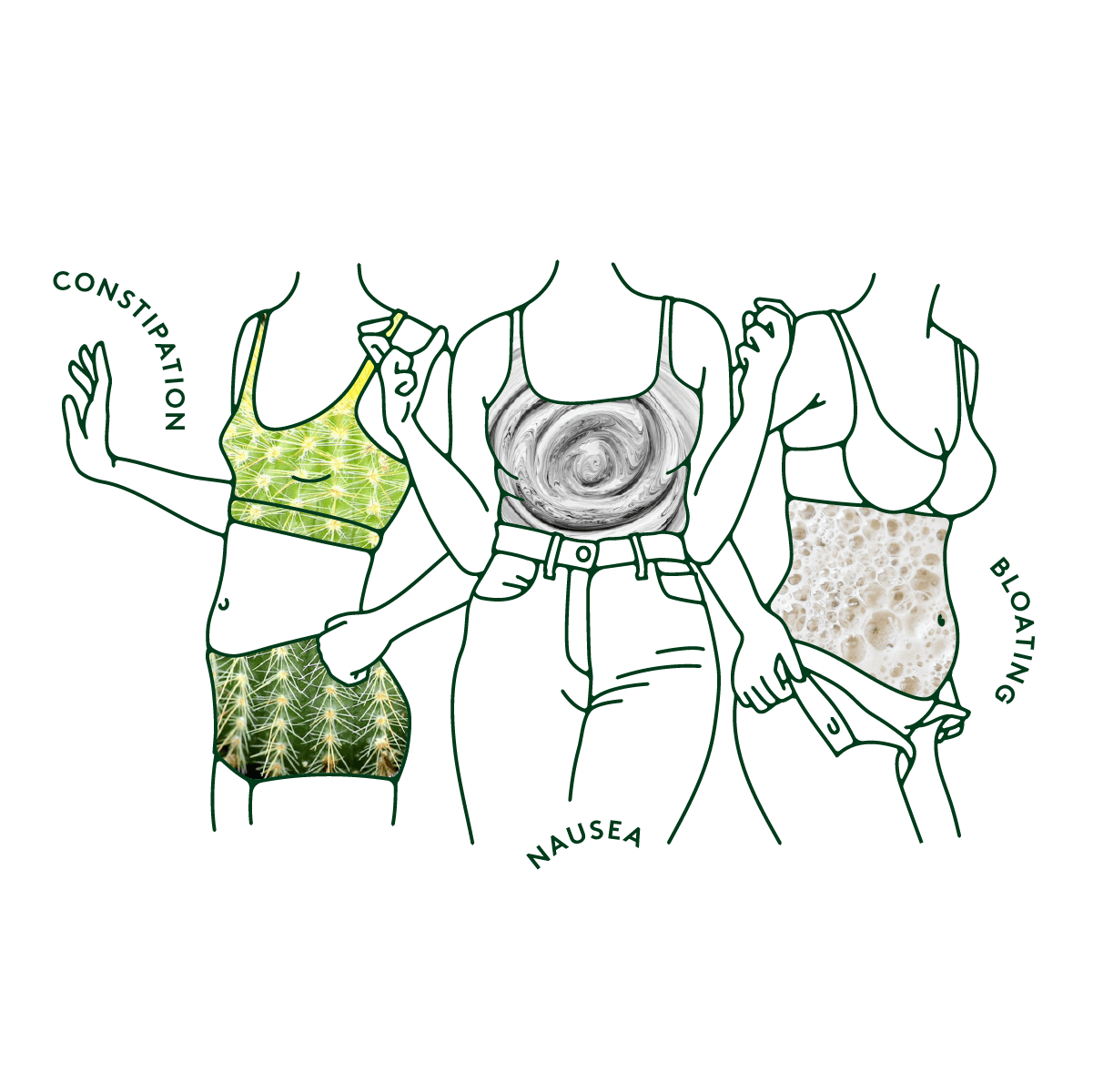
“Many people notice bloating, constipation, diarrhea, nausea, or cravings around their period,” says Alexa Ryan, Naturopathic Practitioner & Clinical Nutritionist. Hormone changes can intensify these symptoms, especially if the gut microbiome is imbalanced.
Prostaglandins, chemicals that trigger uterine contractions, also affect digestion. If your gut microbiome is off, cramps and diarrhea can happen at the same time.
Vaginal symptoms include cyclic vulvovaginitis, a monthly flare of burning, itching, or stinging caused by hormone changes or microbiome shifts. This condition is now seen as an immune–microbiome condition, not just “hormone sensitivity.”

Period pain has often been dismissed as “just part of having a uterus,” but research shows it doesn’t have to be this way. Supporting your vaginal microbiome may reduce pain beyond using hot water bottles or ibuprofen.
At Twentyeight Health, we believe vaginal and reproductive health deserve attention and innovation. That’s why we’ve partnered with Daye, a company pioneering science-backed vaginal care, to bridge the gap between cutting-edge research and everyday solutions.
If you’re managing a BV or yeast infection, our clinicians at Twentyeight can provide personalized guidance and prescription support. And thanks to our collaboration with Daye, you’ll also have access to products and screenings designed with the vaginal microbiome in mind—from tampons that minimize disruption to your vaginal flora, to ProViotics (Daye’s vaginal- and gut-friendly supplements that support healthy Lactobacillus levels), and at-home Vaginal Microbiome Tests that can help identify imbalances and fertility-impacting pathogens.
Twentyeight Health providers can provide personalized guidance and prescriptions. Through Daye, you’ll also have access to microbiome-friendly tampons, probiotics, and at-home tests to detect imbalances.
Together, Twentyeight Health and Daye are working to move vaginal health out of the shadows—making treatment, testing, and everyday care more affordable, accessible, and stigma-free.
This article was reviewed by Twentyeight Health's clinical team. The information provided in this article is for educational purposes only and does not constitute medical advice, diagnosis, or treatment. This content does not establish a provider-patient relationship. Always consult a licensed healthcare professional regarding any medical concerns.